Turn down the dose
Lower-energy radiation could increase access to common cancer treatment
Every year, more than 200,000 Canadians develop cancer, with radiation therapy recommended for almost half those cases. The research of University of Victoria medical physicist Magdalena Bazalova-Carter is striving to improve access and effectiveness of that vital therapy while reducing its harms.
Radiation requires extremely expensive machines housed in specially built rooms to contain the harmful radiation waves. Unfortunately, both those factors make the treatment very costly, and significantly limit its availability even in middle-income countries.
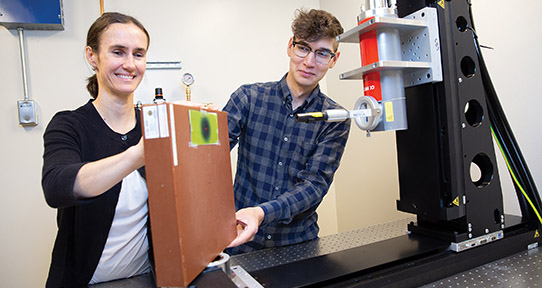
Bazalova-Carter has been working with a US radiation oncologist for the past seven years to develop a new kind of X-ray machine. A prototype resembling a CT scan is being built in Nevada, and a scaled-down version of the machine is being assembled in the UVic lab where Bazalova-Carter conducts her research, the X-ray Cancer Imaging and Therapy Experimental Lab (XCITE).
“What we are proposing is a lower-energy beam that would be delivered from multiple directions at the same time,” says Bazalova-Carter, who is working with graduate student Dylan Breitkreutz on the project. “There’s a larger volume of irradiated tissue but at a lower dose, which should have little impact on healthy tissues, while the tumour receives the same dose.”
Better still, the new machine—which could be commercially available within five years—can be built for a fraction of the cost of high-voltage X-ray equipment. That’s important in light of the need for greater access to radiation therapy around the world, says Bazalova-Carter, Canada Research Chair in Medical Physics.
The high-energy machines currently used for treatment sell for upwards of $5 million each. They require rooms with two-metre-thick concrete walls to protect others from the impact of radiation waves, and a team of engineers to maintain them.
The machine Bazalova-Carter is helping to develop is expected to cost one-tenth of that. Its energy emissions can be contained with nothing more than one-centimetre-thick lead walls.
“It’s not a solution for all radiation therapy cancer treatments, because some tumours are deep in the body and you need that high voltage to reach them. But if you’re talking about lung or breast cancer, it could be a good option,” says Bazalova-Carter.
“Having lower-cost equipment would mean easier access to cancer care all around the world. Even in Canada and the UK, the demand for radiation therapy is not being met. The goal is to end the lineup for radiation, as 10 low-energy machines could be bought for the price normally paid for one, with less space requirements, less concrete, less technical support.”
Bazalova-Carter will also be researching radiation therapy using gold nanoparticles, each smaller than a cell nucleus. The nanoparticles can be injected into cancer patients as a means of concentrating radiation in a tumour while reducing damage to healthy tissue surrounding it. “You target radiation more effectively with less impact on the body,” she says.
Known as “dose-enhanced radiation therapy,” gold nanoparticles are most effective in combination with the low-energy radiation that Bazalova-Carter is studying.
Her research is funded through her Canada Research Chair grant and the Natural Sciences and Engineering Research Council, with support from the Vanier Canada Graduate Scholarship program that funds the work of Breitkreutz, the Canada Foundation for Innovation, and the BC Knowledge Development Fund.
View as PDF (340 KB).
The expense of radiation therapy is a major barrier to accessibility in middle-income countries around the world, where only half of patients with cancers requiring radiation are able to access treatment. In low-income countries, only one in 10 patients who could benefit from radiation therapy are able to access it.
Radiation works against cancer because it interacts with tissue and deposits energy in cancer cells it passes through. That energy kills cancer cells or causes genetic changes that kill cancer, as damaging the DNA of cancerous cells stops them from replicating. However, healthy cells around a tumour are also damaged by radiation, leading to an array of side-effects.
Gold nanoparticles can be injected into patients undergoing radiation therapy with existing equipment to decrease the side-effects of radiotherapy, but they are most effective with low-energy x-rays.
In addition to Dylan Breitkreutz, Bazalova-Carter has two other graduate students engaged in research that builds on her own work: Chelsea Dunning is investigating novel x-ray imaging for accurate detection of gold nanoparticles with a goal of improving cancer diagnosis and radiotherapy; Nolan Esplen is building a device for delivery of microbeam therapy that has been shown to decrease radiation therapy side-effects and promises to be further improved in combination with gold nanoparticle therapy.
Bazalova-Carter was recently awarded the 2018 John Laughlin Young Scientist Award by the American Association of Physicists in Medicine, which recognizes members’ outstanding scientific achievement in medical physics.